
GARDASIL®9 FOR ADULTS
DISCUSS GARDASIL 9
WITH ADULT PATIENTS
THROUGH AGE 45.
You may be able to help protect them
from certain HPV-related cancers.

Millions of men and women aged 45 and under may still benefit from vaccination16
Help protect against certain HPV-related cancers caused by HPV types to which they haven’t yet been exposed.
GARDASIL 9 helps protect against certain cancers caused by 7 HPV typesa
- Cervical
- Vulvar
- Oropharyngeal*
*Continued approval contingent upon confirmatory trial.
- Vaginal
- Anal
aHPV Types 16, 18, 31, 33, 45, 52, and 58.
HPV is not the only cause of these cancers.
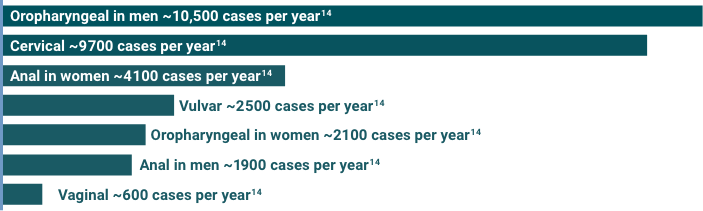
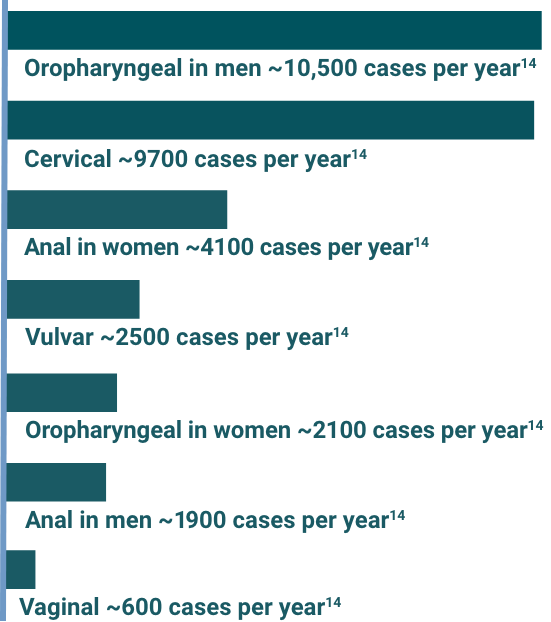
HPV-related oropharyngeal cancers affect men ~5x more than women14,b
CDC-estimated 2012-2016 US incidence model of cancer cases attributed to 7 HPV types (16, 18, 31, 33, 45, 52, and 58)
For most people, HPV clears on its own. But for those who don’t clear the virus, it could cause certain cancers and diseases.10,11,12
~31,400 annual cancer cases in both men and women.14
The oropharyngeal and head and neck cancer indication is approved under accelerated approval based on effectiveness in preventing HPV-related anogenital disease. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
US Cancer Statistics assessed incidence of HPV-associated cancers to estimate the annual number of cancers caused by HPV, overall, and by state in 2012-2016.14
The estimated number of cancers attributable to HPV was calculated by multiplying the average number of HPV-associated cancers by the percentage of cancers diagnosed from 1993-2005 (prevaccine) that were attributable to HPV.14,17
Not all cervical, vulvar, vaginal, anal, and oropharyngeal cancers are caused by HPV.14
Detection of HPV DNA in an HPV study is insufficient to indicate a causal relation with the tumor.17
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Reference
Study Design of 2018 National Health Interview Study (NHIS)
Study Design of 2022 National Immunization Survey (NIS)
Indication for GARDASIL® 9 (Human Papillomavirus 9-valent Vaccine, Recombinant)
GARDASIL 9 is a vaccine indicated in females 9 through 45 years of age for the prevention of cervical, vulvar, vaginal, anal, oropharyngeal and other head and neck cancers caused by human papillomavirus (HPV) Types 16, 18, 31, 33, 45, 52, and 58; cervical, vulvar, vaginal, and anal precancerous or dysplastic lesions caused by HPV Types 6, 11, 16, 18, 31, 33, 45, 52, and 58; and genital warts caused by HPV Types 6 and 11.
GARDASIL 9 is indicated in males 9 through 45 years of age for the prevention of anal, oropharyngeal and other head and neck cancers caused by HPV Types 16, 18, 31, 33, 45, 52, and 58; anal precancerous or dysplastic lesions caused by HPV Types 6, 11, 16, 18, 31, 33, 45, 52, and 58; and genital warts caused by HPV Types 6 and 11.
The oropharyngeal and head and neck cancer indication is approved under accelerated approval based on effectiveness in preventing HPV-related anogenital disease. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
GARDASIL 9 does not eliminate the necessity for vaccine recipients to undergo screening for cervical, vulvar, vaginal, anal, oropharyngeal and other head and neck cancers as recommended by a health care provider.
GARDASIL 9 has not been demonstrated to provide protection against diseases caused by:
- HPV types not covered by the vaccine
- HPV types to which a person has previously been exposed through sexual activity
Not all vulvar, vaginal, anal, oropharyngeal and other head and neck cancers are caused by HPV, and GARDASIL 9 protects only against those vulvar, vaginal, anal, oropharyngeal and other head and neck cancers caused by HPV Types 16, 18, 31, 33, 45, 52, and 58.
GARDASIL 9 is not a treatment for external genital lesions; cervical, vulvar, vaginal, anal, oropharyngeal and other head and neck cancers; or cervical intraepithelial neoplasia (CIN), vulvar intraepithelial neoplasia (VIN), vaginal intraepithelial neoplasia (VaIN), or anal intraepithelial neoplasia (AIN).
Vaccination with GARDASIL 9 may not result in protection in all vaccine recipients.
GARDASIL 9 is contraindicated in individuals with hypersensitivity, including severe allergic reactions to yeast, or after a previous dose of GARDASIL 9 or GARDASIL® [Human Papillomavirus Quadrivalent (Types 6, 11, 16, and 18) Vaccine, Recombinant].
GARDASIL ®9 (Human Papillomavirus 9-valent Vaccine, Recombinant) is contraindicated in individuals with hypersensitivity, including severe allergic reactions to yeast, or after a previous dose of GARDASIL 9 or GARDASIL® [Human Papillomavirus Quadrivalent (Types 6, 11, 16, and 18) Vaccine, Recombinant].
Because vaccinees may develop syncope, sometimes resulting in falling with injury, observation for 15 minutes after administration is recommended. Syncope, sometimes associated with tonic-clonic movements and other seizure-like activity, has been reported following HPV vaccination. When syncope is associated with tonic-clonic movements, the activity is usually transient and typically responds to restoring cerebral perfusion.
Safety and effectiveness of GARDASIL 9 have not been established in pregnant women.
The most common (≥10%) local and systemic adverse reactions in females were injection-site pain, swelling, erythema, and headache. The most common (≥10%) local and systemic reactions in males were injection-site pain, swelling, and erythema.
The duration of immunity of a 2-dose schedule of GARDASIL 9 has not been established.
Dosage and Administration for GARDASIL 9
GARDASIL 9 should be administered intramuscularly in the deltoid or anterolateral area of the thigh.
- For individuals 9 through 14 years of age, GARDASIL 9 can be administered using a 2-dose or 3-dose schedule. For the 2-dose schedule, the second dose should be administered 6–12 months after the first dose. If the second dose is administered less than 5 months after the first dose, a third dose should be given at least 4 months after the second dose. For the 3-dose schedule, GARDASIL 9 should be administered at 0, 2 months, and 6 months.
- For individuals 15 through 45 years of age, GARDASIL 9 is administered using a 3-dose schedule at 0, 2 months, and 6 months.
Before administering GARDASIL 9, please read the Prescribing Information. The Patient Information also is available.
